Case Quiz (March 2023)
A 12-year-old female with a past history of bilateral sensorineural hearing loss had symptoms of headaches, intermittent fevers, body aches, and weakness 2 months prior to admission. She recalled a sensation of her “clothes feeling like they were stinging her body”. Two months prior to admission, the working diagnosis was a viral illness. One month prior to admission, she experienced significant weight loss (5.5 kg), decreased appetite and nearly daily fevers. She also recalls feeling worsened muscle aches until
the point of being unable to walk without assistance 1 week prior to admission. Dyspnea, both at rest and with exertion, increased 1 month prior to admission.
She was evaluated in the ER for pulmonary embolus and CT angiogram chest was normal. A serum chemistry was not performed at the time, but urinalysis showed a pH of 7, proteinuria and microscopic hematuria. She was then discharged home.
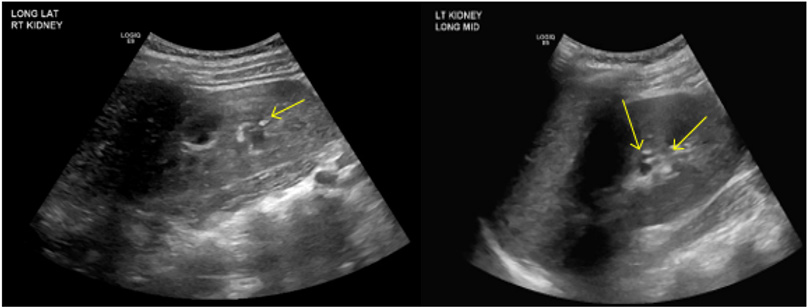
A few days later, blood work was performed at her primary pediatrician’s office, prompting admission for severe hypokalemia and a metabolic acidosis. Upon admission, laboratory findings included elevated ESR, anion gap 7 (plasma CO2 9 mmol/L, primary process with respiratory compensation), hypokalemia, serum creatinine 0.9 mg/dl, normocytic anemia, urine pH 7. Renal U/S revealed echogenic kidneys with punctate, echogenic non-shadowing foci in collecting system bilaterally, suggestive of nephrocalcinosis (Figure).
The patient initially received parenteral electrolyte repletion with improvement in her electrolyte derangements. Her work up was normal for complements, antiphospholipid antibodies, ANCA vasculitides antibody panel, dsDNA, anti-Smith antibody and RNP antibodies. Her coagulation panel and thyroid function studies were also
normal. She underwent infectious work-up including blood cultures, respiratory viral panel, HIV and hepatitis C testing, all of which were negative. Her initial electrocardiogram showed a prolonged QTc that was followed and normalized with correction of her electrolyte abnormalities. She was found to have a normocytic anemia with hemoglobin of 9.5 g/dL on admission associated with reticulocytosis and a positive fecal occult blood.
After her electrolytes stabilized, she underwent an upper and lower GIT endoscopy. The endoscopy was significant for several oozing gastric ulcers, but otherwise unremarkable.
A diagnostic work up was done.
Case Answer (March 2023)
Sjogren syndrome presenting with distal renal tubular acidosis (dRTA) Sjögreńs syndrome (SS) is a chronic progressive autoimmune disease primarily involving exocrine glands with varying degrees of systemic involvement, which can include severe interstitial lung disease, cutaneous vasculitis, peripheral neuropathy, and hematologic complications such as lymphoma. Tubulointerstitial nephritis (TIN) may be a manifestation of renal involvement in primary SS.
This patient had dRTA (metabolic acidosis with ormal anion gap, hypokalemia, urine pH 7 and nephrocalcinosis). The systemic manifestations the patient presented with points to secondary dRTA mostly autoimmune disease.
Salivary gland biopsy was done and showed lymphoplasma cytic infiltrates, which appeared to meet the proposed criteria for Sjogren’s syndrome. Based on immunohistochemistry staining, it did not appear to be secondary to IgG4-releated disease or sarcoidosis. She was thus started on prednisone therapy and transitioned to enteral electrolyte repletion.
After initiation of prednisone, her symptoms began improving
