Case Quiz (November 2020)
A 9-year-old girl presented with abdominal pain, poor appetite, fatigue, and a weight loss of 4.5 kg since her last pediatric appointment, 3 months earlier. She denied joint pain, rashes, hematuria, and pulmonary symptoms. She was previously healthy and had no family history of autoimmune disease. Bilateral conjunctival injection, decreased bowel sounds, and bilateral cervical lymphadenopathy were noted on physical examination.
Her visual acuity was 6/6 in each eye. There was normal pupilary reaction. Slit-lamp examination was significant for 1+ injection with ciliary flush, 4+ fine cell, 2+ flare, anterior vitreous cell spillover, and one posterior synechiae in the left eye. There were no keratic precipitates or iris nodules in either eye. Dilated fundus examination was normal.
Laboratory values revealed serum creatinine 2.1 mg/dl and mild eosinophilia (4.4%). Her ESR was 95 mm/hour with elevated CRP. Urinalysis showed 2+ glycosuria, sterile pyuria, and elevated β2 -microglobulin (β2 -m) at 4324 µg/l. Further workup was negative, including angiotensin converting enzyme, lysozyme, quantiferon gold, rheumatoid factor, antinuclear antibody, antineutrophil cytoplasmic antibody profile, and HLA-B27 serotyping. Complement levels were in the normal range.
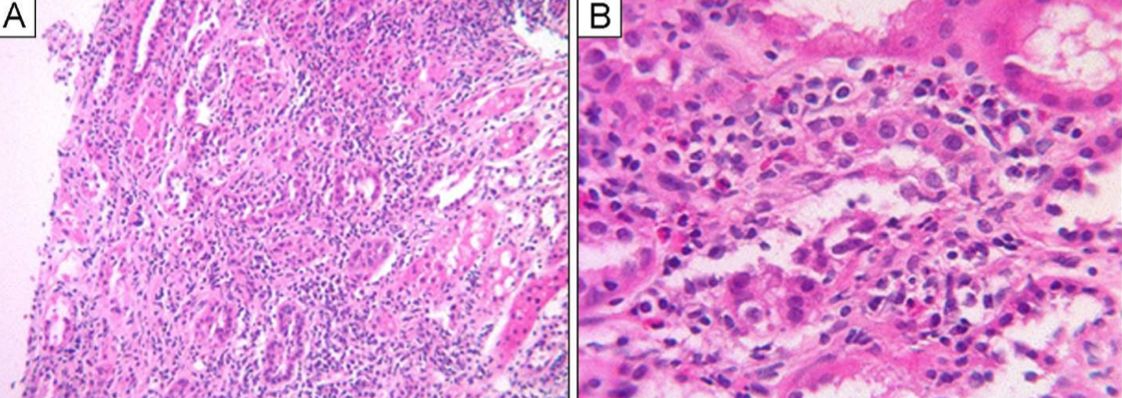
Computed tomography of the chest revealed pulmonary nodules with a halo sign and non-necrotizing granulomatous inflammation (Figure). Due to elevated creatinine in the setting of lung nodules, the patient underwent a renal and pulmonary biopsies (figures below)

Case Answer (November 2020)
Tubulointerstitial nephritis and uveitis (TINU). Renal biopsy revealed revealed marked acute tubulointerstitial nephritis with eosinophils. Lung biopsy revealed revealed non-necrotizing granulomatous inflammation, with negative staining for acid-fast bacilli and fungal organisms.
The differential diagnosis for concurrent uveitis and nephritis includes JIA, TINU, and sarcoidosis. In this case, uveitis and nongranulomatous AIN fulfills the diagnostic criteria of TINU. The pathogenesis of TINU is currently unknown, but some clinical and immunologic similarities suggest a relationship with sarcoidosis. Occasionally sarcoid uveitis (19% of cases) depicts a nongranulomatous pattern. This introduced the possibility that TINU and sarcoidosis are not separate clinical entities but rather exist on a spectrum.
